Patients in England are being put at risk because of the unacceptably poor service they receive from GPs, MPs say. The House of Commons Health Committee blamed the government’s failure to tackle doctor shortages, which had led to a decline in the traditional GP-patient relationship. Seeing a GP should not be like booking an Uber driver, the MPs said.

The warning comes just weeks after ministers launched a drive to improve access to GP services. Last month, Health Secretary Thérèse Coffey promised same-day appointments for those that need them, alongside a guarantee no one would wait longer than two weeks.
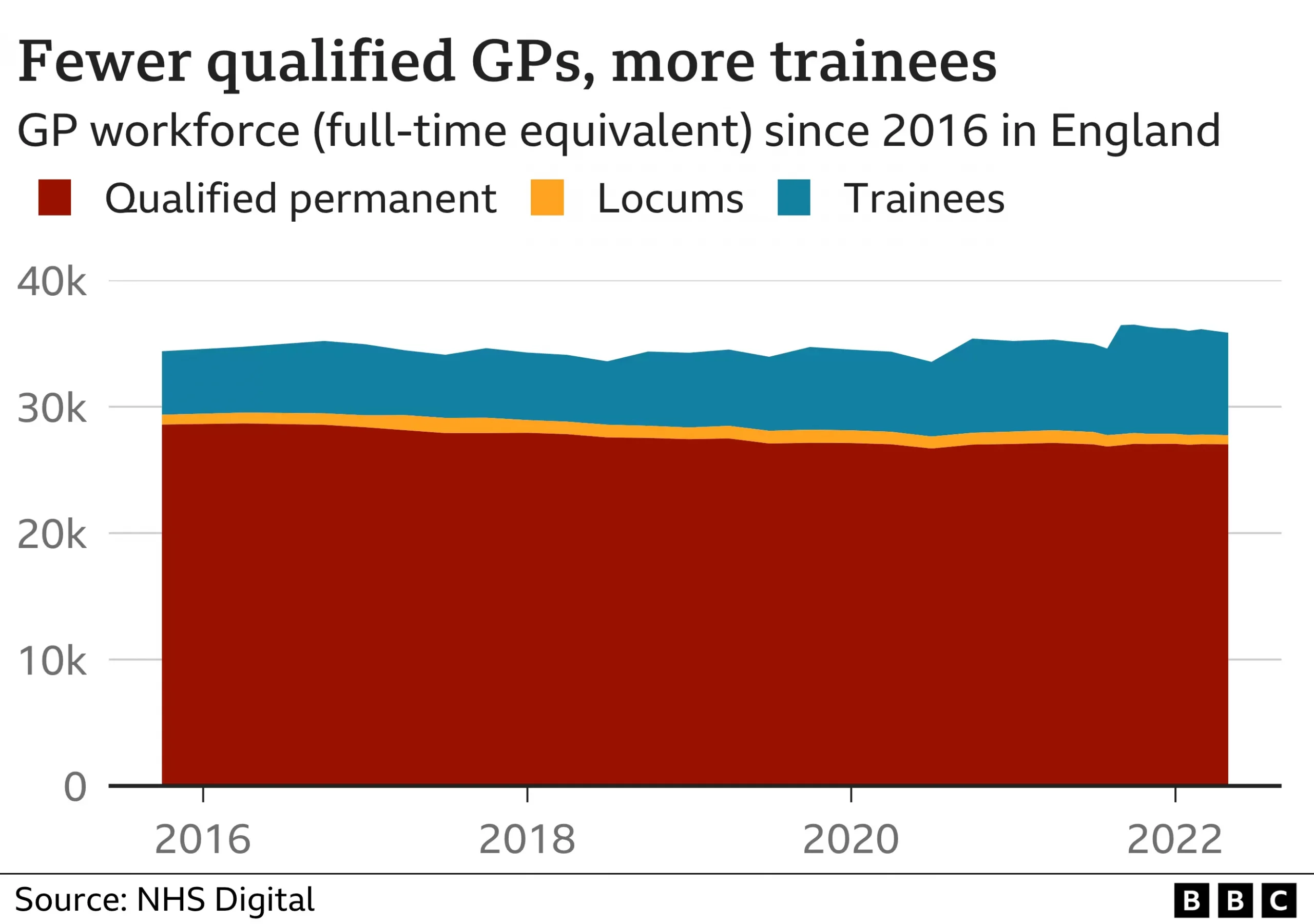
Rules were relaxed so extra funding could be used to recruit non-GP staff, such as senior nurses – as well as asking pharmacists to take on more work to free up appointments – as the government is struggling to achieve its goal of recruiting an extra 6,000 GPs in this Parliament. But the cross-party group of MPs said more needed to be done. And continuity of care – seeing the same GP – was essential to spotting the signs of illnesses early and keeping people healthy and out of the hospital. Committee member Rachael Maskell said: “The important relationship between a GP and their patients is in decline. “Seeing your GP should not be as random as booking an Uber with a driver you’re unlikely to see again. “General practice is in crisis with doctors demoralised and overworked.”
Appalling and Impersonal – The Experience of Patients
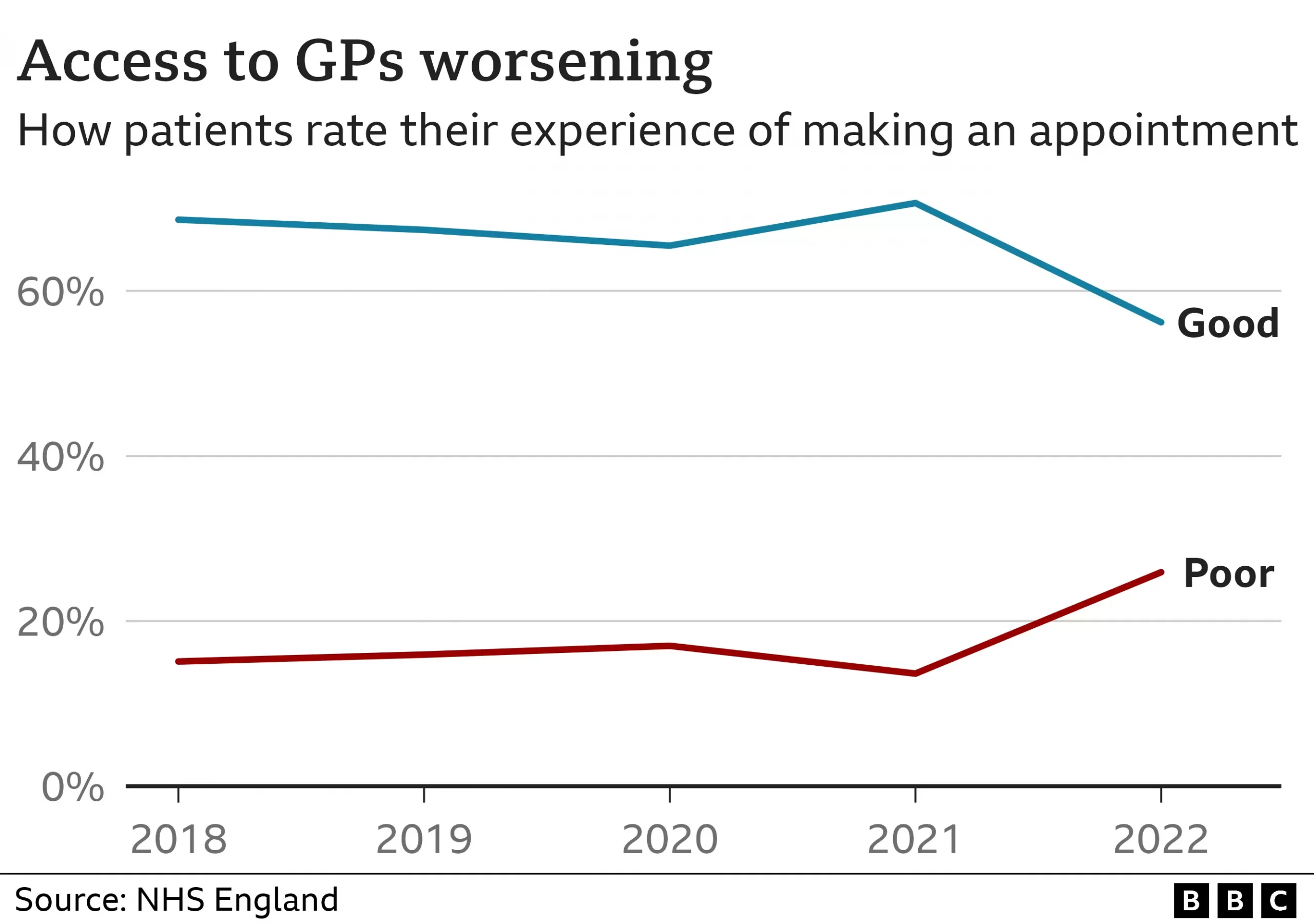
Surveys show a sharp decline in the experience of people trying to see a GP. Alex Boys took his grandmother to an urgent care centre last month after being told it would take three weeks to see her GP. “My gran had a very simple medical complaint to do with her toes,” Alex says. “It seemed like a minor issue – but because my gran is 93, with any medical complaint the anxiety she feels is very real for her.”
Amina Harun, who lives in London with her husband and two children, says her experience of using a GP practice has been “appalling”. Her practice has had to rely on locums, she says, and the service is “impersonal”. “I’ve had terrible experiences with my GP and still continue to have bad experiences,” Amina says. “You can’t call to book appointments and have to do everything via an online app. “This is not good for anyone that is vulnerable and unable to book via phone. “The phone lines are always busy or there’s usually a long wait.”
The committee called for a return of personal lists, so each patient is assigned an individual GP, alongside an expansion of GP training places. By 2027, 80% of GP practices should be using personal lists, it said, and 100% by 2030. An analysis by the Nuffield Trust think tank earlier this year for BBC News found a two-fold variation in the number of patients per GP across different areas of England. And the committee said the poorest areas, which tended to have the fewest doctors and highest levels of ill health, needed more funding.
Prof Martin Marshall, who chairs the Royal College of GPs, said: “The report recognises what the college has been saying for many years – that GPs and our teams are working under unsustainable workforce and workload pressures and this is impacting on the care we are able to deliver to patients. “We need to see urgent action taken.”
![]()





