Health bosses are warning of major disruption and pressure on the NHS in England, as the hot weather combines with the latest junior doctors strike. British Medical Association members will walk out for 72 hours from 07:00 on Wednesday. It is the third strike in the pay dispute and is expected to lead to the cancellation of routine care. And with the heat placing extra demands on accident-and-emergency units, bosses urged people to use services sensibly.

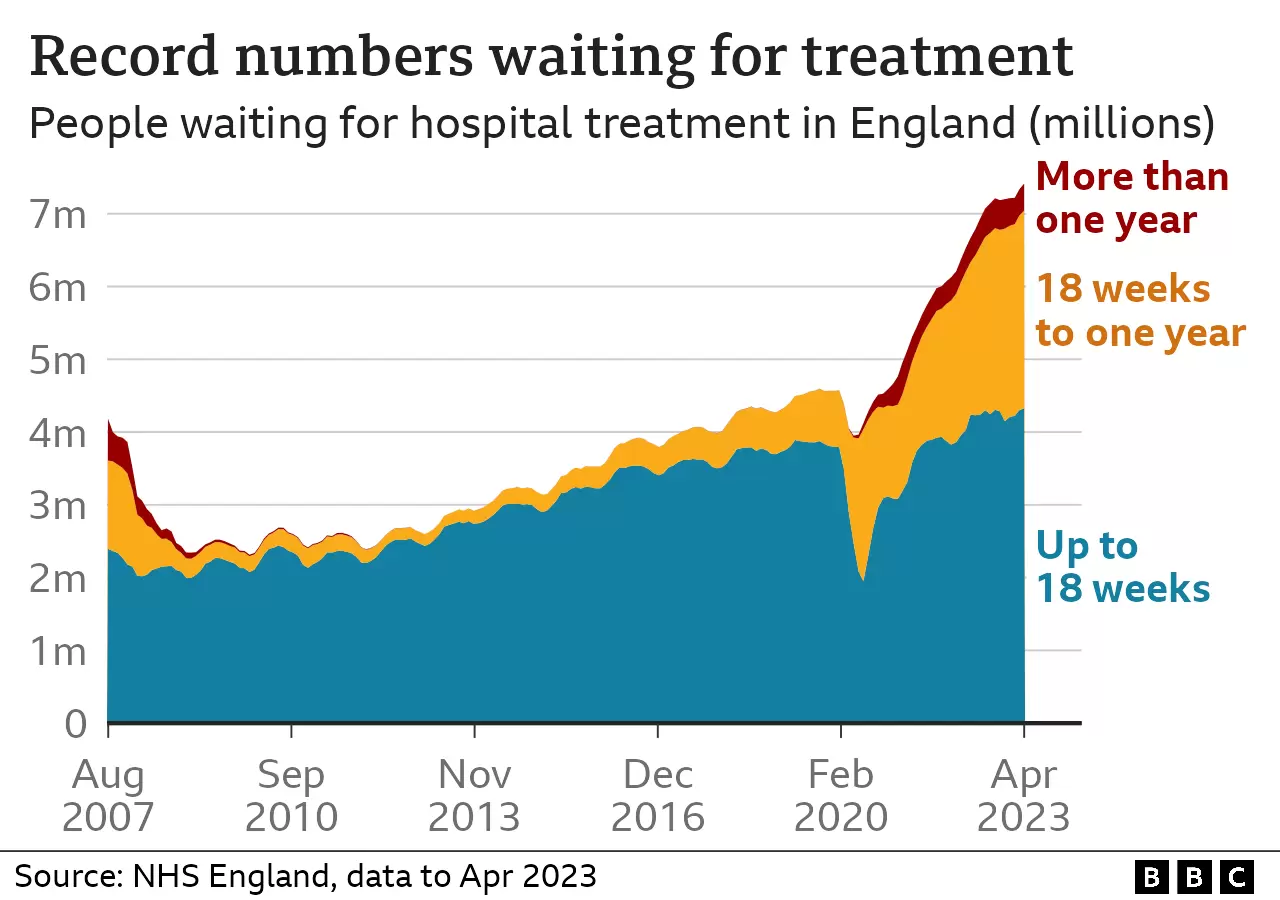
Rory Deighton, of the NHS Confederation, which represents health bosses, said a particular challenge this time was “securing the level of consultant cover” – because of the amount consultants were asking for overtime payments – creating uncertainty over how many appointments would need to be postponed. The four-day April walkout saw about 196,000 hospital appointments and treatments postponed. And the hospital waiting list, growing since the start of the pandemic, has now hit a record 7.4 million people. “Each wave of strikes chips away at the NHS’s resilience, impacting on staff, internal relationships and their ability to deliver on government pledges to reduce the elective backlog,” Mr Deighton said.
‘Significant disruption’
NHS England medical director Prof Stephen Powis said the strike would have an “enormous impact”. “The NHS is facing significant disruption this week, with a three-day strike that is set to be exacerbated by the ongoing hot weather,” he said. “Emergency, urgent and critical care will be prioritised this week but some patients will unfortunately have had their appointments postponed – if you haven’t been contacted to reschedule, please do continue to attend your planned appointment. “As ever, use 999 and A&E for life-threatening emergencies – and NHS 111 online for all other health conditions.” While hospitals are expected to bear the brunt of the disruption, community services, including GPs, will be much less affected.
‘Grossly unfair’
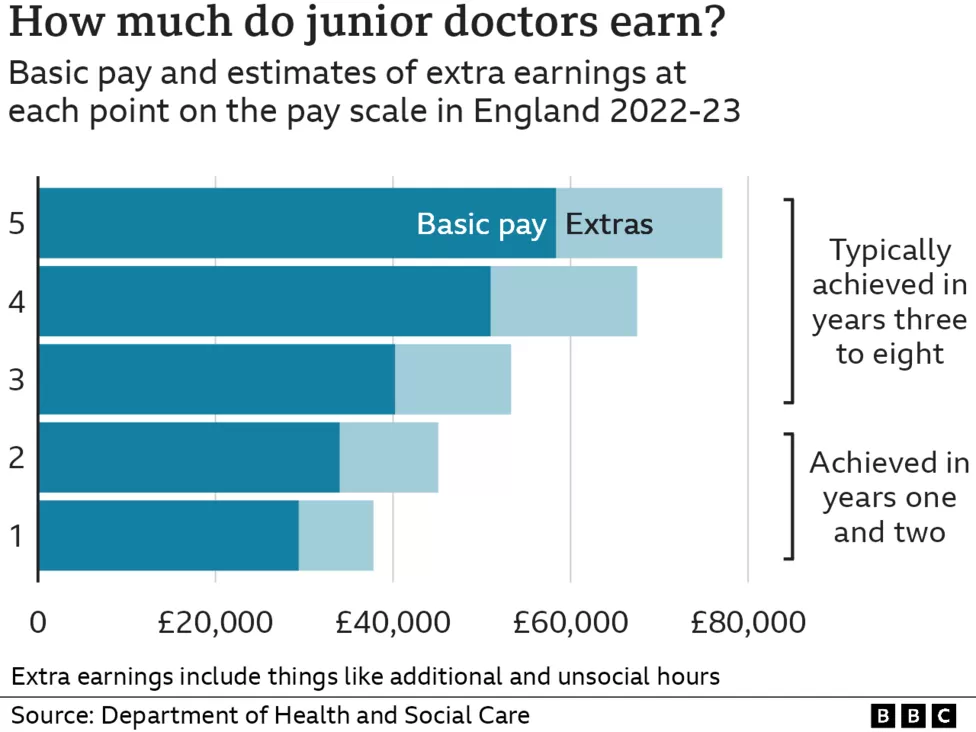
In his second year after medical school, Dr Tom Corkery-Bennett, works an average of 48 hours a week, in the A&E at Royal Berkshire Hospital, but can put in up to 60 and regularly receives messages asking if he can take on extra shifts. What has happened to pay was a major factor in the staffing shortages, the 26-year-old said, and “grossly unfair”.
“The resilience in the system is so low – staffing levels are skeletal,” Dr Corkery-Bennett said. “There is very often situations where doctors call in sick for a nightshift and there’s no cover available. “It means there’s a large number of patients without a doctor to cover them and care is really put in jeopardy. “One doctor will cover the work of two or three doctors if there’s no contingency plan in place, which very often happens, and that’s unsafe.”
Junior doctors want a 35% pay hike to make up for 15 years of below-inflation rises. In talks last month, the government offered an extra 5%, which Health Secretary Steve Barclay called “fair and reasonable”, adding the “extremely disappointing” walkout would put patients at risk. But BMA junior-doctor leader Dr Vivek Trivedi said the offer “beggars belief” given inflation had reached double-digits this year.
‘Properly Valued’
“Junior doctors are in despair at this government’s refusal to listen,” Dr Trivedi said. “We have made clear that junior doctors are looking for the full restoration of our pay. “The NHS can only function with a workforce that is properly valued.” This walkout affects services in England only – but junior doctors in Scotland have this week announced they too will be going on strike, after a vote by BMA members. A strike ballot for consultants in England is also being held. And Royal College of Nursing members are voting on whether to continue their industrial action, after joining the minority of health unions to have rejected the government’s offer of 5% plus a one-off payment of at least £1,655.
![]()





